Built to Last: Your Lifelong Blueprint for Strong Bones
John: Welcome, everyone. Today, we’re building a foundation for a topic that supports our entire lives, quite literally: bone health. It’s something most of us take for granted, like the sturdy frame of a house, until a crack appears. We often think of bone issues as a problem for the distant future, but the reality is that the habits we build today are the bedrock of our skeletal strength for decades to come.
Lila: That’s a great way to put it, John. I have to admit, when I hear “bone health,” my mind immediately jumps to my grandmother worrying about osteoporosis. It feels like a concern for people over 70. Is that a common misconception? Are younger people really at risk?
John: It’s an incredibly common misconception, and a dangerous one. Think of your bones like a savings account for strength. You spend your childhood and young adult years making deposits, building up what’s called ‘peak bone mass.’ This is the maximum strength and density your bones will ever achieve, and for most people, that peak happens around age 30. After that, you start making slow withdrawals. The more you “deposit” in your youth, the more you have to draw upon as you get older.
Lila: A “bone bank account”—I love that analogy! So, it’s not about suddenly getting weak bones when you’re old; it’s about how well you built them up and maintained them throughout your entire life. That completely changes the perspective from a problem to prevent into a lifelong project.

Basic Info: The Framework of Your Life
John: Exactly. It’s a proactive project, not a reactive panic. The core issue is that bone loss is silent. You don’t feel your bones getting weaker day by day. That’s why osteoporosis is often called the “silent thief”—it gradually steals bone density over many years without any symptoms. For many, the first sign that something is wrong is a sudden, unexpected fracture from a minor fall or even a strong sneeze.
Lila: A sneeze? That’s terrifying. It really highlights how fragile bones can become. So, what is osteoporosis, exactly? Is it just “weak bones,” or is there more to it?
John: In simple terms, osteoporosis literally means ‘porous bone.’ Imagine a honeycomb. A healthy bone has small, dense holes. With osteoporosis, those holes become much larger, making the bone’s structure weak, brittle, and highly susceptible to fractures. It’s a formal medical condition diagnosed based on a measurement called Bone Mineral Density (BMD), which we can talk more about later.
Lila: And this is why the **risk of fracture increases as you age**? Because that gradual “withdrawal” from the bone bank has been happening for decades?
John: Precisely. **Aging is associated with a decline in BMD, increasing the risk of osteoporosis and fractures.** It’s a natural process, but the rate of that decline can be dramatically accelerated by poor lifestyle choices or slowed down by good ones. The goal isn’t to stop aging—it’s to uncouple aging from fragility.
Supply Details: The Building Blocks of Bone
Lila: Okay, so let’s talk about building that strong “bone bank account.” What are the essential “deposits” we need to be making, especially in our younger years?
John: The two undisputed superstars of bone health are Calcium and Vitamin D. They are the Batman and Robin of skeletal maintenance. Calcium is the primary mineral that makes up the actual structure of your bones and teeth. Over 99% of your body’s calcium is stored in your skeleton.
Lila: So, it’s the bricks in our biological house. But I hear a lot about Vitamin D, too. How does that fit in?
John: If calcium is the bricks, Vitamin D is the construction foreman who tells the body what to do with them. You can consume all the calcium in the world, but without sufficient Vitamin D, your body can’t absorb it effectively from your gut into your bloodstream to be used by your bones. They work as a team. This is why a chronic deficiency in Vitamin D can lead to softened bones and an **increased risk of fracture**.
Lila: Where do we find these? I know dairy is big for calcium, but what are some other great sources? And for Vitamin D, is sunlight really enough?
John: Excellent questions. For calcium, think beyond milk.
- Dairy: Yogurt, cheese, and kefir are fantastic.
- Leafy Greens: Collard greens, kale, and spinach are good sources.
- Fish: Canned sardines and salmon (with the bones) are calcium powerhouses.
- Fortified Foods: Many plant-based milks (almond, soy, oat), orange juice, and cereals are fortified with calcium.
- Other Sources: Tofu, beans, and almonds also contribute.
For Vitamin D, sunlight is the best natural source, as it triggers production in your skin. However, factors like your location, skin tone, season, and sunscreen use can limit production. So, dietary sources are also critical: fatty fish like salmon and mackerel, egg yolks, and fortified foods are your best bets. Many people, especially in less sunny climates, may need a supplement to reach optimal levels.
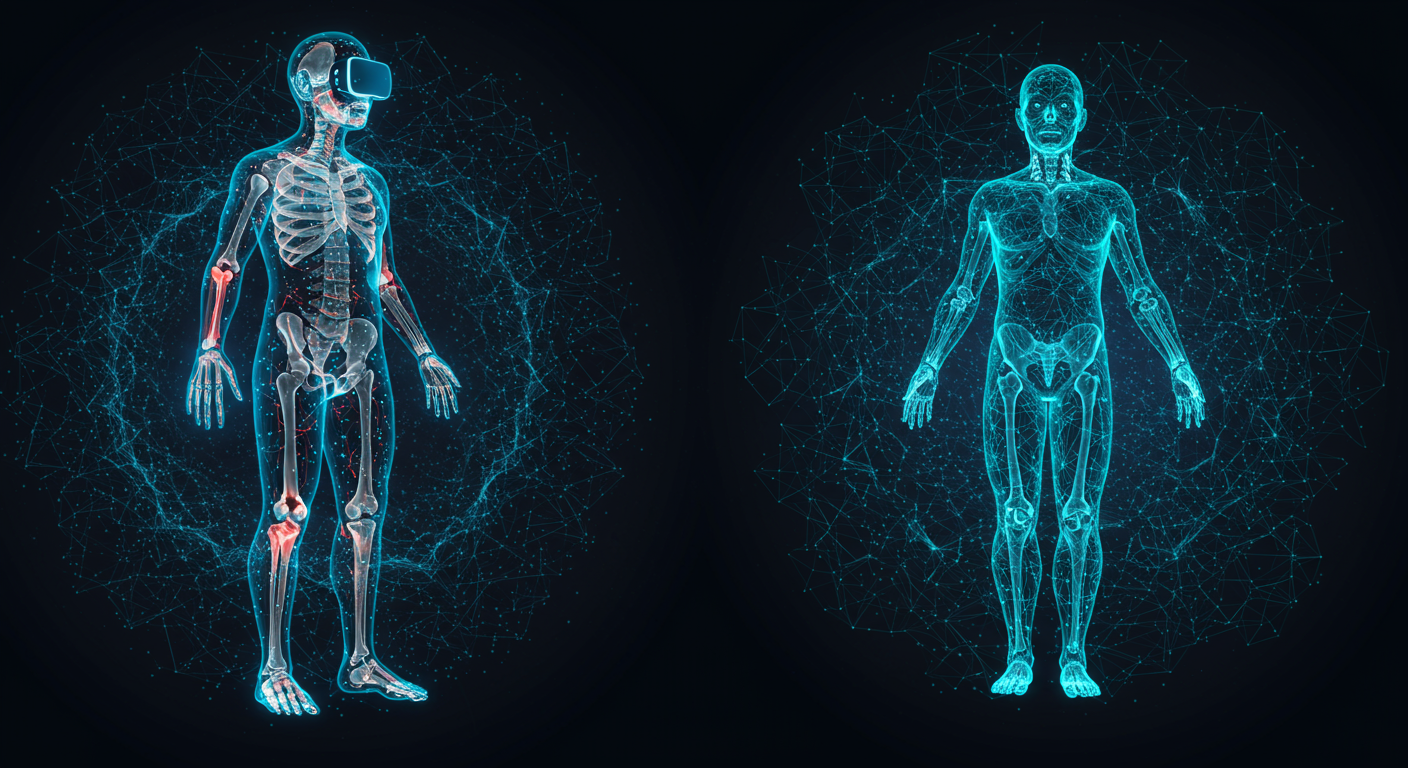
Technical Mechanism: The Constant Remodeling
Lila: You mentioned bones are constantly changing. It’s not like they just grow until we’re 30 and then slowly dissolve. What’s happening on a microscopic level?
John: That’s the fascinating part. Your skeleton is a dynamic, living tissue that is constantly undergoing a process called remodeling. Think of it as a perpetual renovation project run by two types of specialized cells:
- Osteoclasts: These are the “demolition crew.” They break down and resorb old, worn-out bone tissue.
- Osteoblasts: These are the “construction crew.” They follow the osteoclasts, laying down new, strong bone matrix to replace what was removed.
In your youth, your osteoblasts (builders) are more active than your osteoclasts (demolishers), leading to a net gain in bone mass. This is how you build up to your peak.
Lila: So, after our peak around age 30, the balance shifts? The demolition crew starts working a bit faster than the construction crew?
John: Exactly right. The activity of the osteoclasts begins to outpace the osteoblasts, leading to a gradual, net loss of bone. This is a normal part of aging. However, in osteoporosis, this process is dramatically accelerated. Hormonal changes play a huge role here, which is why bone loss often speeds up significantly for women after menopause due to the drop in estrogen, a hormone that helps protect bones. But it’s crucial to remember this isn’t just a women’s issue. Men are also at significant risk, though it typically manifests about a decade later. In fact, about **one in five men over the age of 50 will suffer a bone fracture due to osteoporosis**.
Lila: That’s a staggering statistic. It seems so unfair that our body’s own maintenance process eventually starts working against us. It makes the idea of maximizing those early “deposits” even more critical.
Team & Community: You Don’t Have to Build Alone
John: You absolutely don’t. Managing bone health is a team sport. Your first and most important team member is your primary care physician. They can assess your personal risk factors, discuss your diet and exercise, and decide if and when you need a bone density screening.
Lila: What is a bone density screening? Is it a complicated procedure?
John: Not at all. The gold standard is a DEXA scan, which stands for Dual-Energy X-ray Absorptiometry. It’s a simple, painless, and quick scan—like a low-dose X-ray—that measures the mineral density of your bones, typically at the hip and spine. The results tell your doctor if you have normal bone density, low bone mass (often called osteopenia, a precursor to osteoporosis), or full-blown osteoporosis. It’s a key tool for early detection.
Lila: So your team could also include a radiologist who reads the scan. Who else might be on this “bone health team”?
John: Depending on your situation, you might also work with a rheumatologist or endocrinologist (doctors specializing in bones and hormones, respectively), a physical therapist to design a safe and effective exercise program, and a registered dietitian to fine-tune your nutrition. But the “team” extends beyond medical professionals.
Lila: I see what you mean. It’s also about your community. A workout buddy to keep you motivated for weight-bearing exercise, family members who join you in eating healthier meals, or even support groups for people managing osteoporosis. That community support can be just as crucial as the medical advice.
Use-Cases & Future Outlook: Putting Knowledge into Action
John: Let’s get practical. The most powerful “use-case” for all this knowledge is adopting healthy habits today. It boils down to two main pillars: diet, which we’ve touched on, and exercise. But not just any exercise will do. For bones, you need to create impact and stress, which signals to those osteoblast cells to get to work building more bone.
Lila: So, swimming, while great for cardio, isn’t the best for bones because the water supports you? What kind of exercises are we talking about?
John: Correct. You need two key types of exercise:
- Weight-Bearing Exercise: This is any activity where your feet and legs support your body’s weight. Think high-impact activities like running, jumping, and dancing, or low-impact ones like brisk walking and using an elliptical machine. This directly stresses the bones in your lower body and spine.
- Muscle-Strengthening Exercise: This is resistance training. When your muscles pull against your bones, it stimulates bone growth. This includes lifting weights, using resistance bands, or doing bodyweight exercises like push-ups and squats. This is crucial for strengthening bones in the upper body, like the wrists and spine.
A combination of both is the ideal strategy to **support bone health at every stage of life**.
Competitor Comparison: Choosing Your Strategy
Lila: When we think about strategies, it seems there’s a choice between the lifestyle approach—diet and exercise—and the medical approach, like medications. How do these compare? Is one better than the other?
John: They aren’t competitors so much as partners. Lifestyle is the non-negotiable foundation for everyone, at every age. You simply cannot build or maintain healthy bones without adequate nutrition and the right kind of physical activity. It’s the first line of defense and the primary method of prevention.
Lila: And where do medications come in?
John: Medications are typically reserved for individuals who have already been diagnosed with osteoporosis or are at very high risk of fracture. They are a treatment, not a universal preventative measure. There are several classes of drugs. Some, like bisphosphonates, work by slowing down the osteoclasts (the demolition crew), thereby reducing bone loss. Others work by stimulating the osteoblasts (the construction crew) to build new bone. The choice of medication is a very personal one made between a patient and their doctor, based on their specific DEXA scan results, fracture history, and overall health profile.
Lila: So it’s not an either/or situation. If someone needs medication, they still absolutely need to continue with the diet and exercise strategy to get the best results. The lifestyle habits make the medication more effective.
John: That’s the perfect way to summarize it. You can’t just take a pill and continue a sedentary lifestyle with a poor diet and expect to have strong bones. You must **adopt healthy habits today to maintain bone strength as you age**; it’s the core principle that underpins everything else.
Risks & Cautions: The High Cost of Neglect
John: We’ve alluded to the risks, but it’s important to be explicit. The primary danger of poor bone health is, of course, fractures. But not all fractures are created equal. The most common and debilitating osteoporosis-related fractures occur in specific sites.
Lila: I’ve seen those Apify results. They keep mentioning the hip, spine, and wrist. Why those specific locations? For example, **wrist fractures occur most commonly at age 50-60 years**. Why then?
John: The wrist fracture is often one of the earliest signs. It typically happens from a FOOSH injury—a “Fall On an Outstretched Hand.” As we get a bit older, our balance might not be what it was, and the first instinct when falling is to put a hand out to break the fall. If bone density has already started to decline, the fragile wrist bones can’t withstand the impact.
Lila: And what about the spine? The search results mention vertebral fractures being common in the 60s and 70s.
John: Spinal, or vertebral, compression fractures are particularly insidious. Sometimes they happen from a fall, but often they can occur without any significant trauma at all—from something as simple as lifting a bag of groceries or even just bending over. The vertebrae in the spine weaken and start to collapse on themselves. This can cause severe back pain, a loss of height, and the stooped posture or “dowager’s hump” we sometimes associate with old age. Many people don’t even realize they’ve had one; they just attribute it to general “back pain of aging.”
Lila: That’s frightening. And the hip fracture is the one everyone fears most, right?
John: Yes. A hip fracture, most common in the 70s and 80s, is often a life-altering event. It almost always requires major surgery and extensive rehabilitation. It can lead to a significant loss of independence, with many patients unable to return to their previous level of mobility. Furthermore, it carries a high risk of serious complications and an increased mortality rate in the year following the fracture. **People with osteoporosis have a greater risk of fractures**, and a hip fracture is the most devastating of them all.
Expert Opinions / Analyses: The Scientific Consensus
Lila: What do the big health organizations, like the World Health Organization or the National Institutes of Health, say about this? Is the advice we’re discussing pretty much the consensus?
John: Overwhelmingly so. The global medical and scientific communities are in strong agreement on the fundamentals. The core message from every reputable health authority is that osteoporosis is a largely preventable disease. They all emphasize the lifelong importance of a balanced diet rich in calcium and vitamin D, combined with regular weight-bearing and muscle-strengthening exercise. They also universally advocate for avoiding negative lifestyle factors.
Lila: What are the big “no-no’s” for bone health?
John: The main culprits that actively harm your bones are:
- Smoking: It’s toxic to your bone-building osteoblast cells and can interfere with calcium absorption.
- Excessive Alcohol Consumption: More than two drinks a day for men or one for women can interfere with the body’s calcium balance and the hormones that protect bones.
- Sedentary Lifestyle: Lack of physical stress on the bones tells your body it doesn’t need to maintain a strong skeleton. It’s the “use it or lose it” principle in action.
- Poor Diet: A diet lacking in key nutrients and high in processed foods deprives your bones of the raw materials they need to stay strong.
The expert analysis is clear: while we can’t stop the clock, **you can maintain your bone health and lessen your fracture risk** significantly by focusing on what you can control.
Latest News & Roadmap: The Future of Bone Health
John: The future is quite promising. Research is constantly evolving. One of the most interesting new frontiers is the distinction between chronological age (your age in years) and biological age (how old your body seems on a cellular level). New research is examining how **biological age, calculated from routine lab tests, predicts 1-year mortality in elderly hip fracture patients better than chronological age**. This could help doctors better tailor post-fracture care to the patients who need it most.
Lila: Wow, so your ‘real’ age matters more than your birthday. What about treatments? Are there new drugs on the horizon?
John: Yes, researchers are always working on more targeted therapies with fewer side effects. There’s a lot of focus on drugs that can more powerfully stimulate the bone-building osteoblasts, potentially even reversing significant bone loss, not just slowing it down. Another area is improving screening. There’s a push to make screening more accessible and to develop better risk-assessment tools that go beyond just a DEXA scan, incorporating genetics and other lifestyle factors to give a more holistic picture of a person’s fracture risk.
Lila: So the “roadmap” is towards more personalized and proactive care? Instead of waiting for a fracture, we’ll be able to identify high-risk individuals even earlier and with greater accuracy?
John: That’s the goal. The future is about precision prevention. It’s about giving people the specific knowledge and tools they need to ensure their skeleton can support a long, active, and independent life. The aim is to make debilitating fractures a rare event, not an expected part of aging.

FAQ: Your Quick Questions Answered
Lila: Let’s do a quick-fire round. I’ll ask some common questions, and you can give us the concise, expert take. First up: I’m over 40, have I missed the boat on building bone mass?
John: Absolutely not. While you may have passed your peak, it is never too late to make a difference. Adopting a bone-healthy lifestyle at any age can slow the rate of bone loss and, in some cases with intensive exercise, even slightly increase density. Most importantly, it will improve your strength and balance, which directly reduces your risk of falling and getting a fracture.
Lila: Are calcium and Vitamin D supplements a good idea for everyone?
John: Not necessarily. The best approach is “food first.” Try to get your nutrients from a balanced diet. If your diet is lacking, or if you have absorption issues or high needs, a supplement might be necessary. But it’s crucial to discuss this with your doctor. Too much calcium from supplements can have risks, so it’s not something to do without medical guidance.
Lila: Does bone health differ between men and women?
John: Yes. Women tend to have smaller, thinner bones and they experience rapid bone loss after menopause. This puts them at a higher risk earlier in life. However, men are by no means immune. As we said, by age 65 or 70, men and women lose bone mass at similar rates. Men’s bone health is a seriously under-discussed public health issue.
Lila: Final question: If I feel fine and haven’t broken any bones, do I still need to worry about this?
John: Yes, a thousand times, yes. That is the entire point. Bone loss is silent. Feeling fine is not an indicator of bone density. The time to “worry”—or better yet, to be proactive—is when you feel perfectly fine. Because **building your bones now will help prevent fractures as you age.** Don’t wait for the alarm bell of a fracture to sound. Start building your foundation today.
Related links
John: It’s been a fantastic discussion, Lila. The key takeaway is simple: your bones are a lifelong investment. The deposits you make through diet and exercise, starting from today, will pay dividends in strength, mobility, and independence for the rest of your life. Don’t let your skeletal health be an afterthought.
Lila: I couldn’t agree more. It feels empowering to know that so much of our future strength is within our control right now. It’s not about fearing old age, it’s about building a body that’s ready to live it to the fullest. Thanks, John.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Do Your Own Research (DYOR).